What is Fertility?
Fertility is defined as the natural capacity to conceive a child. However, fertility does not come easily to everyone. About 11% of couples in the world are facing the issue of infertility—the inability to conceive naturally after one year of unprotected sexual intercourse.
What to Expect?
The obstetrician–gynecologist often is the first health care provider women will seek for evaluation or concerns about fertility. Essential components of an initial workup include a review of the medical history and additional tests as indicated.
Medical History
The first visit with a fertility specialist usually involves a detailed medical history. You will be asked questions about:
Your menstrual period
Abnormal bleeding or discharge from the vagina
Pelvic pain
Any disorders that can affect reproduction such as thyroid disease.
You and your partner will be asked about the duration of infertility and results of any previous evaluation and treatment. You and your partner will also be asked about your Pregnancy history:
Time to pregnancy,
Fertility treatments,
Pregnancy outcome
Delivery route,
Associated complications,
Previous methods of contraception,
Coital frequency and timing
Past surgery (procedures, indications, and outcomes) focused on abdominal and pelvic procedures,
Current medications and supplements, with an emphasis on identifying allergies and
Potential baby unfriendly medications,
Family history of birth defects, early menopause, or reproductive problems
Occupational exposure to known environmental hazards,
Use of nicotine products, alcohol, and recreational drugs.
Female Infertility Causes
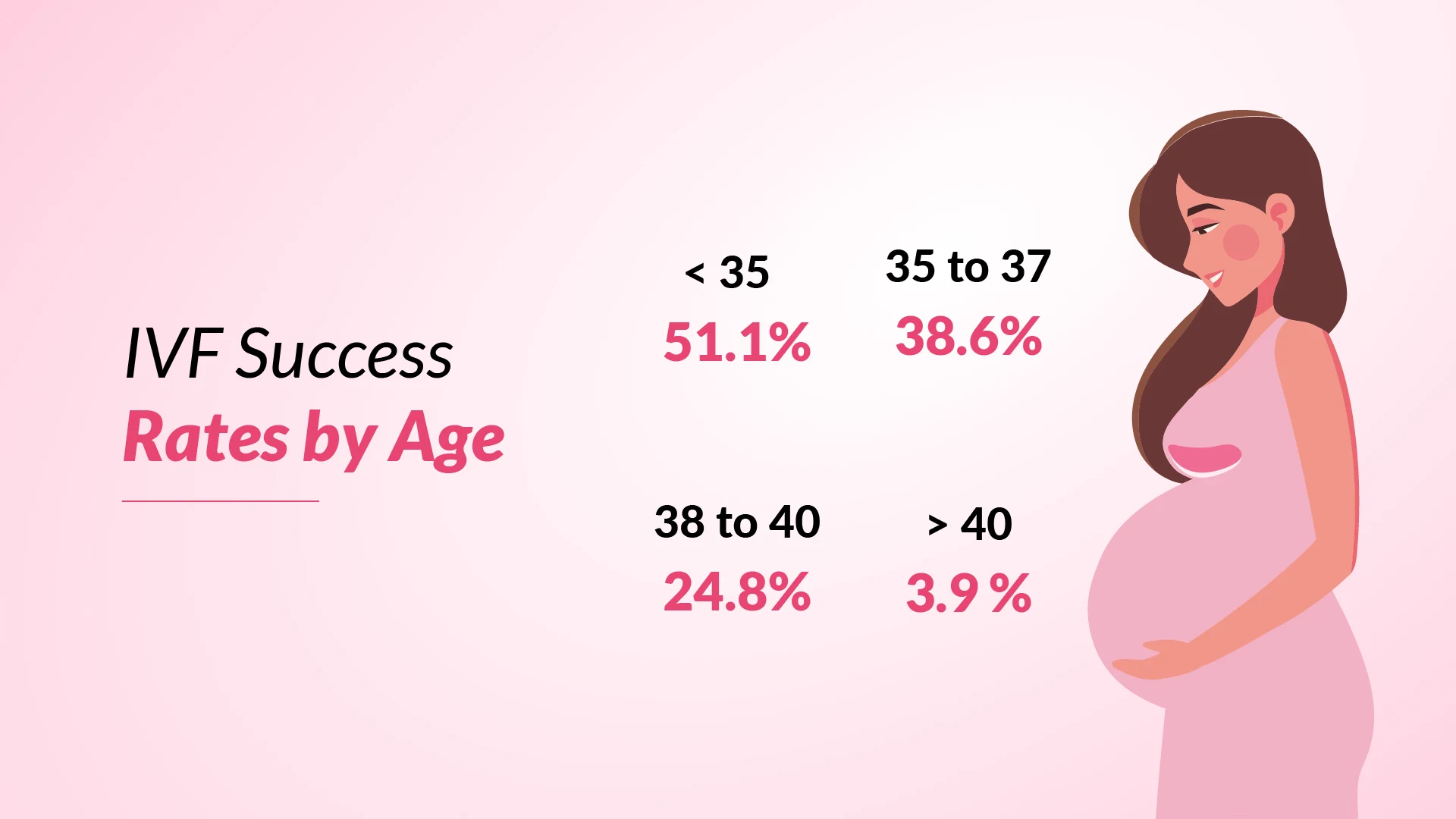
Age: Age is the most important factor which affects a woman’s chances of conception and having a healthy baby. As a woman’s age advances her fertility starts declining since there is a reduction in the quantity and quality of the eggs in the ovaries. A woman’s fertility starts declining in her early 30s and this becomes more rapid after 35 and at age 40 and above there is a very minimal chance of conceiving. The problem lies in the fact that with advancing age there is an increased percentage of chromosomally abnormal eggs. These poor quality eggs results in poor embryo quality which reduces the chance of getting pregnant.

PCOS: PCOS also known as Stein Leventhal syndrome is the most common hormonal endocrine problem with at least 10% of women getting affected. Basically a woman having PCOS do not ovulate every month and hence have an irregular menstrual cycle and there are multiple cysts in the ovaries. If not diagnosed and managed earlier PCOS might lead to several medical complications like insulin resistance, high cholesterol, diabetes, hypertension and heart disease. Women with PCOS have a high testosterone level which leads to hirsutism, male pattern baldness and acne.
Fibroids: Fibroids or leiomyomas or uterine myomas are the most common non-cancerous growth in women which develops in and around the uterus or womb. The cause of fibroids is not very well understood but it does have a genetic predisposition. Early onset of puberty, obesity, hormonal problems may also be some other causes of fibroid. Some women with fibroids have no signs and symptoms, while some have severe pain, heavy and prolonged menstrual bleeding etc. There are a few women who complain of frequent urination, abdominal swelling, painful intercourse etc.

Hormonal Imbalance: There are a number of hormonal imbalances which lead to infertility problems in women. Irregular menstrual cycles, absence of periods, lesser or heavier than normal periods are all indications of some abnormality in the FSH/LH and estradiol hormones. Excessive weight gain, abnormal hair growth, hair loss, acne etc are also due to hormonal imbalance. PCOS is an example of such a hormonal disorder which is one of the most common causes of infertility. Other examples of such imbalance are hypothyroidism, hyperprolactinemia, luteal phase defect or low progesterone and premature ovarian failure. There are a number of reasons which cause hormonal imbalance in our body; some of them are stress, poor nutrition, body fat, lifestyle choices, menopause, genetic predisposition etc.
Tubal Block: Fallopian tube damage is a major cause of female infertility accounting to almost 20% of all infertility cases. When there is block or damage in the tube the egg and the sperm cannot meet and so there is no fertilization. Many women who are trying to conceive are not even aware that their tubes are damaged as there are no obvious symptoms. The most common cause for tubal damage is pelvic inflammatory diseases with gonorrhoea or Chlamydia, tuberculosis of the genital tract, endometritis/peritonitis/appendicitis and HIV infection. The various tests to diagnose tubal blockage are HSG, SSG/SIS, HyFoSy/HyCoSy and laparoscopy.

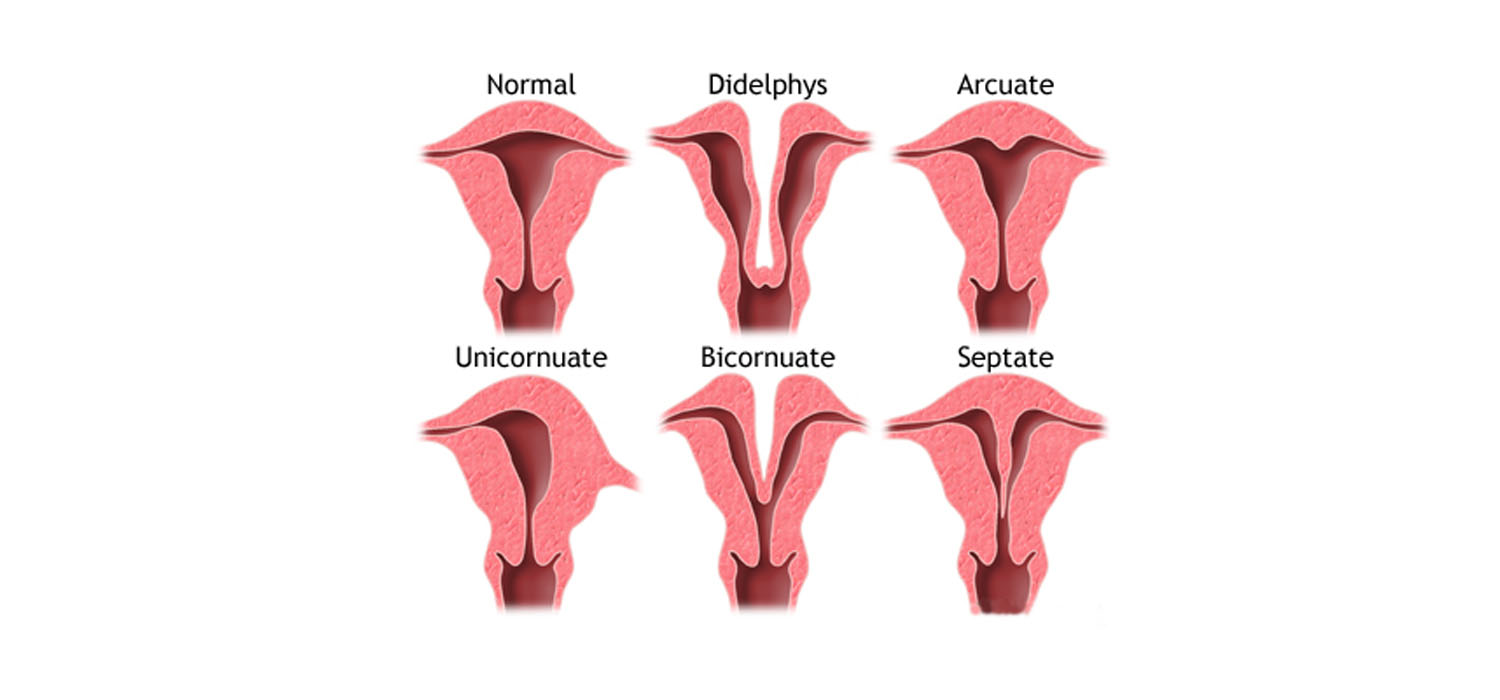
Uterine Abnormalities: Uterine abnormalities are associated with infertility, ectopic pregnancy, recurrent pregnancy loss and various other obstetric complications. The investigations carried out in order to diagnose any uterine abnormality are HSG, SSG/SIS or ultrasound scan and also invasive procedures like the hysteroscopy and laparoscopy. Uterine abnormalities will include intrauterine adhesions as well as growths like fibroids and polyps for which the treatment is surgical removal with very minimal risk.
Tests
The infertility workup includes laboratory and imaging tests.
For the female partner, tests will focus on:
Testing the ovarian reserve
Testing for ovulatory function
Looking for structural abnormalities
Testing for Tubal patency
Ovarian Reserve Tests
The reproductive potential of the ovaries or a woman’s supply of eggs, termed ovarian reserve, represents the number of eggs available for potential fertilization at that point in time and may be assessed by two tests:
Blood tests (AMH)
Ultrasonography (AFC:Antral Follicle Count)
The presence of decreased ovarian reserve predicts future response to ovarian stimulation during IVF. The results of ovarian reserve tests should be considered in the context of the patient’s age. Although there are no definitive criteria for diminished ovarian reserve, the following values may be considered consistent with diminished ovarian reserve:
Antimüllerian hormone (AMH) value less than 1 ng/mL
Antral follicle count less than 5–7 and
Follicle-stimulating hormone (FSH) greater than 10 IU/L between cycle days 2–5.
A history of poor response to in vitro fertilization stimulation (fewer than four eggs at time of egg retrieval)
Ovulatory Dysfunction
Clinical history can be used to assess ovulatory cycles because most ovulatory women will have regular menstrual cycles every 25–35 days accompanied by premenstrual symptoms. However, up to one third of women with normal menstrual cycles are anovulatory; therefore, confirmation of ovulation should be considered. Most commonly this is done by folliculometry or tracking the growth of egg/eggs via transvaginal sonography. Anovulation may be related to obesity, pituitary dysfunction, PCOS, and other causes. Polycystic ovary syndrome is the most common cause of not ovulating. Thyroid disease and increased levels of a hormone called prolactin can cause ovulatory dysfunction. Thus, measuring TSH and prolactin in the empty stomach is important for women presenting with inability to conceive.
Testing for Uterine Factor or Structural abnormalities (SIS - Saline Infusion Sonography)
Uterine factors associated with infertility include:
Polyps
Scarring in uterus(synechia)
Anomalies of shape of uterus (septate uterus)
Fibroids. Fibroids with a surgically modifiable effect on fertility include those having a cavity-distorting component.
Testing for Tubal Factor
Tubes are portals through which sperm travels to meet the egg for fertilization. In case of tubal block, fertilization and pregnancy is not possible and IVF would be an option for these couples especially if associated with suboptimal semen parameters.
Saline infusion sonography (SIS) is the visualization of the uterus ultrasonographically with the infusion of fluid through a very thin tube placed in the womb via the cervix without putting you to sleep. An extension of SIS, hysterosalpingo-contrast sonography (Hy-CO-Sy) determines tubal patency with the use of a special contrast dye.
