What is ICSI?
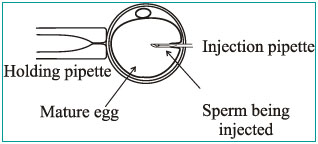
ICSI or Intracytoplasmic sperm injection is a laboratory procedure developed to help infertile couples undergoing assisted reproduction due to male factor infertility. ICSI, a form of micromanipulation, involves the injection of a single sperm directly into the cytoplasm of a mature egg (oocyte) using a glass needle (pipette).
This process increases the likelihood of fertilization when there are abnormalities in the number, quality, or function of the sperm. ICSI is generally unsuccessful when used to treat fertilization failures that are primarily due to poor egg quality.
How is ICSI done?
Before ICSI can be done, mature eggs must be retrieved from the female partner during a standard IVF cycle. The male partner's semen sample is prepared in the lab to isolate as many healthy moving sperm as possible. After allowing the eggs to rest for 4-6 hours following their removal, the tight outer coating of cells (cumulus) is removed from each egg. Only then can we be sure the egg is mature enough to undergo ICSI.
Immature eggs cannot be injected. However, they can be incubated for a further 4-18 hours and reassessed. If they mature during that time and sperm is still available, they can undergo delayed injection. Fertilization rates with delayed injection are not as good as with usual ICSI techniques.
What are the indications for ICSI?
- Very low numbers of motile sperm.
- Severe teratospermia (abnormal sperms).
- Problems with sperm binding to and penetrating the egg.
- Antisperm antibodies thought to be the cause of infertility.
- Prior or repeated fertilization failure with standard IVF methods.
- Frozen sperm limited in number and quality.
- Obstruction of the male reproductive tract not amenable to repair. Sperm may then be obtained from the epididymis by a procedure called microsurgical epididymal sperm aspiration (MESA), or from the testes by testicular sperm aspiration (TESA).
- Embryo biopsy for genetic testing of embryos can only be done if a sigle sperm is used to fertilize the oocyte thus requiring ICSI.
What are the fertilization rates with ICSI?
Fertilization occurs in 50% to 100% of injected eggs. The ICSI process may damage a small percentage of eggs but that usually happens in eggs which are bad anyways. The fertilized egg may fail to divide, or the embryo may arrest at an early stage of development. Approximately 40% of all ICSI cycles performed result in a live birth, which is comparable to rates seen with traditional IVF. Younger patients may achieve even more favourable results. Factors such as poor sperm / egg quality and advanced maternal age may result in lower rates of success.
Are there any complications with ICSI?
ICSI does not increase the incidence of multiple gestations as compared to standard IVF. To date, there is no convincing evidence that the incidence of birth defects is any different with ICSI or IVF as compared to those children born to other parents of similar age and health. This is an area of ongoing investigation. Because some causes of male infertility are familial and are related to genetic problems, male offspring might have reproductive problems as adults. Despite these concerns, ICSI is a major advance in the treatment of severe infertility.


